
Testing for COVID-19 is technical, expensive and complicated — particularly in Alaska, with its remote, far-flung communities and overlapping systems of tribal and private health care.
That complexity and scope make it hard to assess just how well Alaska has performed in its testing program, as officials tout statistics that show the state is the nation’s most tested.
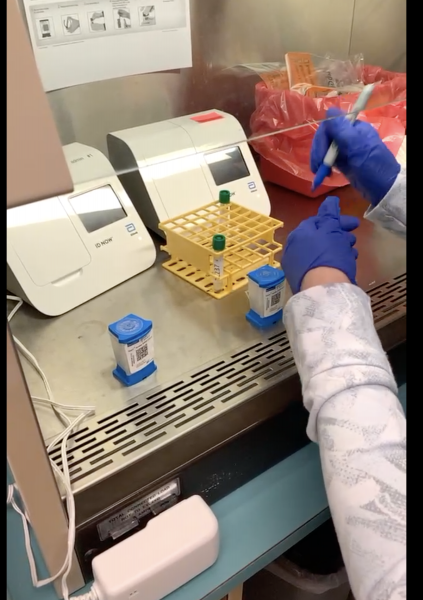
But Alaska’s use of one particular type of rapid testing machine, the Cepheid, offers a window into both state and national successes and failures when it comes to COVID-19 testing. The machines themselves are scattered widely across the state, and some have been essential in protecting communities from an influx of summer workers and visitors — but many other Cepheids are going unused because of an extremely tight supply of the testing cartridges needed to run them.
Cepheid machines are known for being both sensitive and reliable, and a federal shipment of supplies directed to fishing towns around the state has allowed providers to test tens of thousands of samples on a rapid basis. That’s helped reduce the need to fly samples to state labs on the road system, where tests can take several days to come back.
In communities that weren’t designated for the federal supplies, though, other Cepheid machines are sitting largely idle because of the lack of the cartridges. Some health-care providers have even sent letters appealing directly to the company that manufactures them, to no avail.
State and federal officials point out that Alaska continues to perform well when it comes to the sheer number of tests conducted. Its rate of positive tests continues to sit below 2%, and overall turnaround times for testing sit at roughly three days for state labs, health-care facilities and private labs — significantly less than in some virus-plagued areas of the country, where results can take a week or more to come back.
Read full COVID-19 coverage from Alaska Public Media
The Cepheids are just one of the many types of machines used to test for COVID-19, and providers say they’re filling in gaps by flying out samples and using another type of machine, the Abbott ID Now, for rapid tests.
But in contrast with the Cepheid machines, some of which can run 16 tests an hour, the Abbotts only process one at a time. And some providers don’t trust them because of preliminary reports that they don’t detect every case of COVID-19.
They argue that the cartridge shortage for the Cepheid machines has made it more difficult to detect the virus quickly and efficiently, particularly in some of the larger Alaska communities off the road system. And experts say that this uneven distribution of tests is happening across the country at the state and local level, reflecting the absence of a coordinated federal testing program.
Instead, the Trump administration has called on states to develop their own testing plans. The federal government has supported states in their efforts to maximize testing within the constraints of national and global supply chains, but it hasn’t developed a strategy to fix the underlying problems with those supply chains that are limiting access, said Dr. Tom Tsai, a surgeon and assistant professor at the Harvard T.H. Chan School of Public Health.
“What Alaska is experiencing, in some ways, is a microcosm of what the country is experiencing,” said Tsai, who worked in the Obama administration. “Each of the states is essentially left to its own devices in terms of how to allocate scarce testing resources. And that also then gets carried down into individual cities and individual health-care systems.”
The different experiences of two coastal Alaska communities underscores the difference in access to the rapid Cepheid tests.
In the Prince William Sound fishing town of Cordova, population 2,000, the vast majority of COVID-19 tests are processed locally and quickly, said Dr. Hannah Sanders, chief executive of the town’s small hospital. About half of those are run on a Cepheid machine on loan from the state.
Rapid testing is particularly important in Cordova because of its fishing industry, with seafood processing employees working and living in close quarters. Cordova’s hospital has just 23 beds and no intensive care unit, while COVID-19 outbreaks on Alaska fishing vessels and at other processing plants around the state have infected dozens of workers at a time.
“The spread can happen pretty quickly in those congregate settings,” Sanders said. “So it’s a very important test, to catch those early.”
Cordova’s testing program has benefited from an unusual level of federal support for testing in Alaska’s commercial fishing industry, which came at the direction of Mark Meadows, President Donald Trump’s chief of staff.
Earlier this year, the Trump administration shipped Alaska 40,000 of the highly-coveted cartridges used to run each Cepheid test, which in turn were dispensed largely to fishing towns around the state.
“Let’s just say if it weren’t fishing season, you’d probably get a thousand a month,” said Admiral Brett Giroir, assistant secretary for health and the Trump administration’s COVID-19 testing czar. “This was a significant commitment to Alaska. I don’t think we’ve made this type of commitment to any other major metroplex or state.”

Giroir, in a phone interview, rejected the idea that Alaska communities would have received better access to testing through a more centralized national program.
If the federal government had prioritized mass production of a single, standardized COVID-19 test, for example, rather than supporting states’ and cities’ use of different types of privately manufactured testing machines around the country, Alaska would have been “up a creek, without a paddle,” Giroir said.
“Because we wouldn’t have the diversity in platforms that we would need to support a New York City,” he said, “and still be able to support Bristol Bay for fishing.”
Nonetheless, even with the tens of thousands of extra cartridges provided by the federal government, access to the rapid Cepheid tests across the state has been inconsistent, according to health-care providers and local officials.
Alaska Gov. Mike Dunleavy’s administration said it could not provide a breakdown of how the Cepheid tests have been distributed, but some details emerged through interviews.
In Juneau, for example, rapid testing looks strikingly different than it does in Cordova.
The city-owned hospital’s two Cepheid machines in Juneau have the capacity to run about 200 rapid tests each day. But for now, they’re operating at just a tiny fraction of their maximum, processing no more than 10 rapid tests daily.
That’s roughly the same amount as in Cordova, even though Juneau’s population is more than 10 times as large.
Juneau’s Cepheid cartridges, obtained directly from the company, are primarily reserved for screening people in the hospital at risk of infecting health-care providers, said Robert Barr, a local emergency response official.
Hundreds of other samples, including those from non-hospitalized people experiencing COVID-19-like symptoms, must be flown to state labs each week. Results take three to five days to come back, which, in the case of positive tests, delays the tracking of sick people’s contacts.
“We do put in requests to the state for additional Cepheid test kits,” Barr said. “But generally, our requests go unfulfilled.”
So do other requests from Alaska health care providers.
In Anchorage, the tribally-run Alaska Native Medical Center has a Cepheid machine that could run 500 rapid tests every 24 hours. But the cartridge crunch has limited it to processing fewer than 200, total, since July 1.
At Kenai Peninsula’s largest hospital, in Soldotna, a Cepheid machine sat largely unused for most of the spring and summer, until Alaska’s Congressional delegation earlier this month intervened with Trump administration officials to help secure additional weekly shipments of 4,000 Cepheid cartridges for the state.
Since then, about 100 of the cartridges have been distributed to the Soldotna hospital each week, said spokesman Bruce Richards. Previously, nearly all samples had to be driven 150 miles to Anchorage for testing at the state lab, with results not coming back for two to three days. And most are still being processed that way.
In Bethel, the hub community for dozens of Southwest Alaska villages, tribal health care provider Yukon-Kuskokwim Health Corp. appealed directly to the company that makes the Cepheid machines.
In a letter last month, it asked for 2,500 cartridges “to help prevent community spread of the disease in one of the most remote, economically depressed and medically underserved areas of the United States.”

So far, it’s received no response.
The Cepheid machines are one of two brands of rapid testing machines used widely in Alaska, also known as “point of care” tests. The other point-of-care machine is the Abbott ID Now.
Earlier this year, the federal government sent 15 Abbotts to each state, with the exception of Alaska, which got 50 because of its remoteness. And now there are 150 or more Abbotts scattered across rural parts of the state, said Dr. Bob Onders, medical director at the Alaska Native Tribal Health Consortium.
The Abbott machines can produce results in fewer than 15 minutes, and they’ve been instrumental in allowing rural providers to test frequently and quickly at places like airports, according to Onders. They’ve also been easier to get supplies for, and have “filled a very important role in the tribal health system,” Onders said.
But while the Abbott machines have been used widely, providers cited two big reasons they still want broader access to cartridges for the Cepheid machines.
One is that early in the pandemic, the Food and Drug Administration warned that “early data” suggested that Abbott machines were failing to detect all cases of COVID-19. One study, before it was peer-reviewed, said the Abbotts missed the virus in 15% of specimens that contained it.
Many Alaska providers say they’ve since become more comfortable using the Abbott machines — particularly when testing people who aren’t living or working in a place where they risk spreading the virus to large numbers of people, like a seafood processing plant or a nursing home. But others say they still don’t want to depend on the Abbott results and prefer the Cepheid machines for rapid testing.
The second problem with the Abbott devices is that they run just one sample at a time, making them challenging to use for large-scale testing.

The Cepheid machines come in different sizes, but some can run as many as 16 samples at once. If there were adequate cartridges for them, they could help bridge what Onders describes as a “missing link” in Alaska’s COVID-19 testing system: higher-volume testing in rural hub communities, which otherwise have to fly large numbers of samples to state labs.
It’s been “extremely frustrating,” Onders said, “to have analyzers that could be helping the communities, and we can’t run them” because of the uneven supply of cartridges.
The Cepheid supply crunch isn’t expected to ease any time soon. Only about 3% of demand for the company’s cartridges is currently being fulfilled nationally, said Coleman Cutchins, a top state testing official.
Officials from Cepheid wouldn’t provide exact figures. But in an interview, Dr. Dave Persing, the company’s chief medical and technology officer and executive vice president, acknowledged that the cartridges are in “very, very short supply.”
Cepheid is making about 2 million tests a month, and producing them “as quickly as we can, as many as we can,” Persing said in a phone interview.
But substantial production increases won’t happen quickly, he added, because “we actually have to build new buildings and manufacture the equipment that’s used to manufacture our cartridges.”
“We’ll be making incrementally more as time goes on,” Persing said. “But the fastest part of the ramp-up has already occurred, and we’ll be making incremental improvements and, hopefully, a second-level ramp some time next year.”
Both Giroir, the federal testing czar, and Cutchins, the state testing official, argued that rapid tests aren’t feasible, or even necessary, for many Alaskans. For people who live in their homes and are following public health recommendations to quarantine while awaiting results, a rapid test doesn’t provide that much value over one that takes a few days to process, they argued.
“If you’re exposed, or you think you’re sick, waiting three days for a test — I know everyone would like to have it in 15 minutes, but just chill out, stay isolated in your home until your test comes back,” Giroir said. “Because we can’t have everything we want right now — this is a historic pandemic.”
Cutchins also noted that in spite of the cartridge crunch for the Cepheid machines, supplies have been much more widely available for the other type of rapid testing machine, the Abbott.
And because of its access to supplies for those two different types of machines, he added, rural Alaska has actually had much better access to testing than many road system communities that have relied on the larger-scale but slower machines at state labs in Anchorage and Fairbanks.
Onders, the tribal health leader, argued that Alaska’s rural, indigenous residents deserve more access to testing and other resources, because data show that minority communities like Alaska Natives, Native Americans and African Americans are getting sick and dying from COVID-19 at disproportionate rates.
“Our advocacy has been that if you want equitable outcomes, you have to have unequal investment,” Onders said. “The populations that may be at the highest risk for bad outcomes, you have to overinvest in them. And testing is a component of that.”
"machine" - Google News
August 26, 2020 at 11:25PM
https://ift.tt/2YC69aF
This machine is a microcosm of Alaska's, and America's, COVID-19 testing successes and failures - Alaska Public Media News
"machine" - Google News
https://ift.tt/2VUJ7uS
https://ift.tt/2SvsFPt
Bagikan Berita Ini














0 Response to "This machine is a microcosm of Alaska's, and America's, COVID-19 testing successes and failures - Alaska Public Media News"
Post a Comment